
The lumbosacral spine is the source of pain, suffering, and disability more frequently than any other part of the body. Pain in the lower back can be managed with computed tomography-guided analgesic interventional procedures, such as periradicular infiltration, percutaneous laser disk decompression, facet joint block, and percutaneous vertebroplasty:
Periradicular Inifitration Nerve root inflammation is responsible for low back pain and sciatica in at least some patients. Periradicular infiltration involves injection of a steroid and an anesthetic into the epidural space at the level of the diseased disk. Addition of a steroid to the anesthetic has been shown to increase the efficacy of periradicular infiltration, probably by decreasing inflammation of the epidural space. The major indications for periradicular infiltration are acute, discogenic low back pain (without nerve paralysis) that is resistant to conventional medical therapy and postdiskectomy syndrome. The procedure is performed on am outpatient basis. The patient is placed prone on the CT table, and a CT scam of the affected level is obtained for precise selection of the needle pathway. After local anesthesia of the skin, a 22-gauge spinal needle is placed near the painful nerve root under CT control. In intracanal infiltration, absence of cerebrospinal fluid is verified by means of aspiration. A long-acting corticosteroid (3.75 mg of cortivazol) is then injected into the epidural space; the steroid solution (2-3 mL) is sometimes mixed with a solution of 0.5% lidocaine (2 mL). Meningitis with neurologic damage (eg, quadriplegia, multiple cranial nerve palsy, nystagmus) can occur after epidural or intrathecal injection of steroids if strict sterility is not maintained. A sterile technique will limit the risk of infection. With precise CT monitoring, accidental intrathecal injection cam be avoided.
Percutaneous Laser Disk Decompression
Percutaneous removal of the nucleus pulposus has been performed with a variety of chemical and mechanical techniques for the past several years. These techniques involve removing all or part of the nucleus pulposus to induce more rapid healing of a diseased disk. Percutaneous nucleotomy is now widely used because it is much less invasive than surgical diskectomy. Traditional surgical therapy of disk herniatiom has the following drawbacks: significant soft-tissue injury, extensive hospitalization, and recovery time of 6 weeks or longer. The most promising method to date in terms of simplicity and minimal invasiveness is percutaneous laser disk decompression (PLDD), which involves the introduction of laser energy into the nucleus pulposus through an 18-gauge percutaneous needle. The advantage of this technique is that the volume and pressure of the diseased disk are reduced without damage to other spinal structures. All percutaneous techniques for removing the nucleus puhposus are based on reduction of the volume of the diseased disk. Ablation of a relatively small volume of the nucleus pulposus results in a significant reduction in intradisk pressure. The indications for PLDD are contained disk herniation at CT or magnetic resonance (MR) imaging combined with positive neurohogic fmdings (leg pain of greater intensity than back pain; positive straight-legraising test; decreased sensation, motor response, and tendon reflex) and failure of 6 weeks of conservative therapy. The contraindications are nerve paralysis, hemorrhagic diathesis, spondylolisthesis, spinal. stenosis, previous surgery at the indicated level, significant psychologic disorder, significant narrowing of the disk space, and an industrial injury with monetary gain. Complications of PLDD performed under CT and fluoroscopic guidance are rare. The major complication of percutaneous mucleotomy is septic diskitis.
Intraarticular Steroid Injection
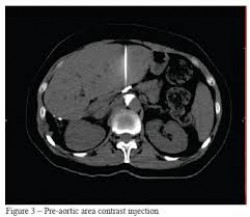
Inraarticular injection of a steroid is performed in patients in whom diagnostic blocks show that facet joints are the source of back pain. Injection of facet joints in the lumbar spine is a simple and safe procedure that can be performed under CT or fluoroscopic control. Degenerative disease of facet joints usually affects multiple levels and both sides; thus, multilevel injection of facet joints (eg, L3-4, L4- 5, and L5-S1) on both sides could be necessary. We perform this procedure under CT guidance. The patient is placed in the prone position on the CT table. CT of the affected level is performed to determine the needle pathway and entry point. A 22-gauge spinal needle is them advanced vertically into each facet joint. Once CT shows that the needle is in the joint, a solution of cortivazol and 0.25% bupivacaine hydrochloride is injected into the joint. Cortivazol is provided in the form of a 1 .5-mL sohutiom (3.75 mg); with the addition of 1 .5 mL of 0.25% bupivacaine hydrochloride, a 3-mL sohution is obtained. The injection is usually performed bilaterally with 1 .5 mL of the solution injected into each side. Complications of lumbar facet joint injection performed with precise needle positioning are rare. Severe allergic reactions to local anesthetics are uncommon. Steroid injection can produce local reactions, which most often occur immediately after the injection. These reactions last 24-48 hours and can be relieved by application of ice.
Percutaneous Facet Joint Denervation
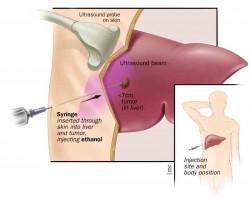
In some patients, facet joint injection produces consistent but temporary pain relief. For these patients, facet joint denervation (rhizolysis) can be consideredThe patient is placed in the prone position on the CT table. A CT scan is obtained at two levels: the superior border of the transverse process below the diseased joint and the superior border of the transverse process above the diseased joint A 22-gauge spinal needle is advanced vertically under precise CT guidance into the internal superior border of each of these transverse processes. Once the needles are in contact with bone and their positioms are confirmed with CT, 1 mL of iohexol (iodine concentration, 240 mg/mL) is injected for prediction of ethanol diffusion and extravascular positioning of the needle tip. The fmal step is injection of 1 .5 mL of 95% ethanol at each level

Leave a Reply
Want to join the discussion?Feel free to contribute!