Radiofrequency ablation (RFA) is a treatment that uses imaging guidance to place a needle electrode through the skin into a liver tumor. High-frequency electrical currents are passed through the electrode, creating heat that destroys the cancer cells. RFA is an effective treatment option for patients who might have difficulty with surgery or those whose tumors are less than one and a half inches in diameter. The success rate for completely eliminating small liver tumors is greater than 85 percent.
Your doctor will instruct you on how to prepare. Inform your doctor if there’s a possibility you are pregnant and discuss any recent illnesses, medical conditions, allergies and medications you’re taking. Your doctor may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners several days prior to your procedure and instruct you not to eat or drink anything for several hours beforehand. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. Plan to have someone drive you home afterward.
What is Radiofrequency Ablation of Liver Tumors?
Radiofrequency ablation, sometimes referred to as RFA, is a minimally invasive treatment for cancer. It is an image-guided technique that uses heat to destroy cancer cells.
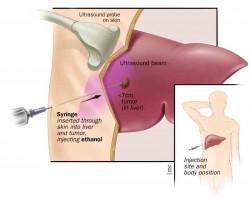
In radiofrequency ablation, imaging techniques such as ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) are used to help guide a needle electrode into a cancerous tumor. High-frequency electrical currents are then passed through the electrode to ground pads placed on the body, creating focal heat that destroys the cancer cells surrounding the electrode.
Microwave ablation, also a minimally-invasive cancer treatment, also uses ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to guide placement of a specialized needle-like probe into a tumor and uses microwaves to heat and destroy it. Microwave ablation is used for the same indications as for RFA. The procedure is typically performed on an outpatient basis or with overnight observation in the hospital with general anesthesia. Microwave ablation has advantages over radiofrequency ablation (RFA), including the ability to treat tumors that are larger and those that are close to major arteries and veins. It can also be used to treat multiple tumors simultaneously. For the patient, microwave ablation offers minimal risk, typically little or no pain and a short hospital stay. The procedure can be repeated if new cancer appears.
Microwave ablation is effective in overcoming the cooling effects of blood flow in the liver, which allows for larger ablation zones than RFA and other heat-based ablation methods.
What are some common uses of the procedure?
Radiofrequency ablation is used to treat many types of liver cancer. The two most common types are:
- hepatocellular carcinoma, which is a primary liver cancer (meaning it begins in the liver).
- colon cancer that metastasizes or spreads from the colon to the liver.
In general, radiofrequency ablation is most effective treating tumors that are less than one and a half inches in diameter. It may be used in addition to chemotherapy or radiation therapy or as an alternative to surgical treatment.
Radiofrequency ablation is a viable and effective treatment option if you:
- are not a good candidate for surgery because your tumor is difficult to reach.
- have other medical conditions that make surgery especially risky.
- would not have enough liver tissue left for the organ to function adequately following the surgical removal of a tumor.
- have liver tumors that have not responded to chemotherapy or that have recurred after being removed surgically.
- you have several small liver tumors that are too spread out to be removed surgically.
How should I prepare?
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as "dye" or "x-ray dye"). Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure.
Prior to your procedure, your blood may be tested to determine how well your kidneys are functioning and whether your blood clots normally.
Women should always inform their physician and x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
You will likely be instructed not to eat or drink anything after midnight before your procedure. Your doctor will tell you which medications you may take in the morning.
You should plan to have a relative or friend drive you home after your procedure.
You may be asked to wear a gown during the procedure.
What does the equipment look like?
The equipment used in this procedure depends on the type of imaging used—magnetic resonance (MR), computed tomography(CT), or ultrasound. Other equipment such as needle electrodes, an electrical generator and grounding pads may also be used.
Radiofrequency equipment
There are two types of needle electrodes: simple straight needles and a straight, hollow needle that contains several retractable electrodes that extend when needed.
The radiofrequency generator produces electrical currents in the range of radiofrequency waves. It is connected by insulated wires to the needle electrodes and to grounding pads that are placed on the patient's back or thigh.
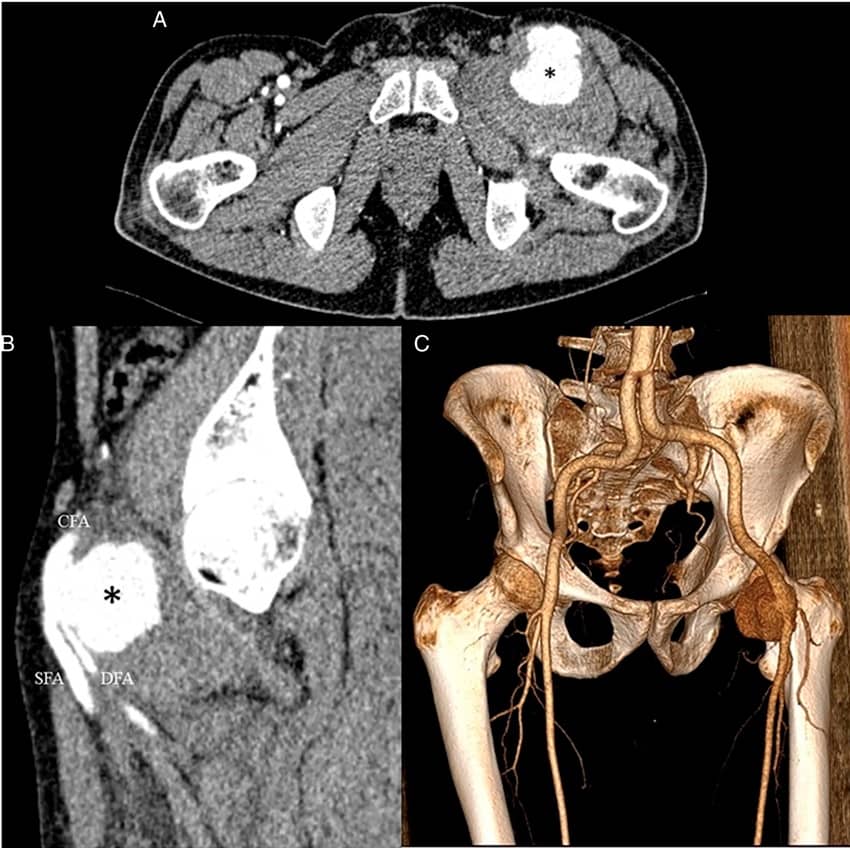
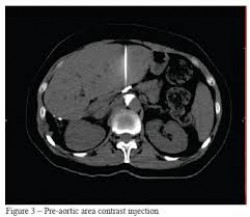
Computed Tomography (CT)
The CT scanner is typically a large, box-like machine with a hole, or short tunnel, in the center. You will lie on a narrow examination table that slides into and out of this tunnel. Rotating around you, the x-ray tube and electronic x-ray detectors are located opposite each other in a ring, called a gantry. The computer workstation that processes the imaging information is located in a separate control room, where the technologist operates the scanner and monitors your examination in direct visual contact and usually with the ability to hear and talk to you with the use of a speaker and microphone.
Ultrasound equipment
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer that is used to do the scanning. The transducer is a small hand-held device that resembles a microphone, attached to the scanner by a cord. Some exams may use different transducers (with different capabilities) during a single exam. The transducer sends out inaudible, high—frequency sound waves into the body and then listens for the returning echoes from the tissues in the body. The principles are similar to sonar used by boats and submarines.
The ultrasound image is immediately visible on a video display screen that looks like a computer or television monitor. The image is created based on the amplitude (loudness), frequency (pitch) and time it takes for the ultrasound signal to return from the area within the patient that is being examined to the transducer (the device used to examine the patient), as well as the type of body structure and composition of body tissue through which the sound travels. A small amount of gel is put on the skin to allow the sound waves to best travel from the transducer to the examined area within the body and then back again. Ultrasound is an excellent modality for some areas of the body while other areas, especially the lungs, are poorly suited for ultrasound.
Magnetic Resonance Imaging
The traditional MRI unit is a large cylinder-shaped tube surrounded by a circular magnet. You will lie on a moveable examination
table that slides into the center of the magnet.
Some MRI units, called short-bore systems, are designed so that the magnet does not completely surround you. Some newer MRI machines have a larger diameter bore which can be more comfortable for larger size patients or patients with claustrophobia. Other MRI machines are open on the sides (open MRI). Open units are especially helpful for examining larger patients or those with claustrophobia. Newer open MRI units provide very high quality images for many types of exams; however, older open MRI units may not provide this same image quality. Certain types of exams cannot be performed using open MRI. For more information, consult your radiologist.
The computer workstation that processes the imaging information is located in a separate room from the scanner.
Other equipment that may be used during the procedure includes an intravenous line (IV), ultrasound machine and devices that monitor your heart beat and blood pressure.
How does the procedure work?
Radiofrequency ablation works by passing electrical currents in the range of radiofrequency waves between the needle electrode and the grounding pads placed on the patient's skin. These currents create heat around the electrode, which when directed into the tumor, heats and destroys the cancer cells. At the same time, heat from radiofrequency energy closes small blood vessels and lessens the risk of bleeding. The dead tumor cells are gradually replaced by scar tissue that shrinks over time.
Ultrasound, computed tomography or magnetic resonance imaging may be used to help the physician guide the needle electrode into the tumor.
How is the procedure performed?
Image-guided, minimally invasive procedures such as radiofrequency ablation are most often performed by a specially trainedinterventional radiologist in an interventional radiology suite or occasionally in the operating room.
Radiofrequency ablation is often done on an outpatient basis.
You will be positioned on the examining table.
You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedation medication can be given intravenously.
The area where the electrodes are to be inserted will be sterilized and covered with a surgical drape.
Your physician will numb the area with a local anesthetic if the procedure is to be done while you are awake. If general anesthesia is used, you will have a breathing tube placed through your mouth and into your trachea after you are asleep. The breathing tube will be connected to a breathing machine while you are asleep.
A very small nick may be made in your skin to make it easier to pass the RFA electrode into your liver.
Radiofrequency ablation is performed using one of three methods:
- Surgery.
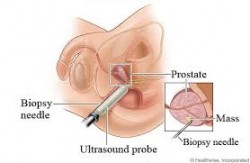
- Percutaneous, in which needle electrodes are inserted through the skin and into the site of the tumor.
- Laparoscopic, in which needle electrodes within a thin, plastic tube is threaded through a small hole in the skin in a procedure called a laparoscopy.
Using imaging-guidance, your physician will insert the needle electrode through the skin and advance it to the site of the tumor.
Once the needle electrode is in place, radiofrequency energy is applied. For a large tumor, it may be necessary to do multiple ablations by repositioning the needle electrode into different parts of the tumor to ensure no tumor tissue is left behind.
At the end of the procedure, the needle electrode will be removed and pressure will be applied to stop any bleeding and the opening in the skin is covered with a dressing. No sutures are needed.
Your intravenous line will be removed.
Each radiofrequency ablation takes about 10 to 30 minutes, with additional time required if multiple ablations are performed. The entire procedure is usually completed within one to three hours.
What will I experience during and after the procedure?
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected. Most of the sensation is at the skin incision site which is numbed using local anesthetic. You may feel pressure when the catheter is inserted into the vein or artery.
If the procedure is done with sedation, the intravenous (IV) sedative will make you feel relaxed and sleepy. You may or may not remain awake, depending on how deeply you are sedated.
If you are put under general anesthesia, your throat may be sore after you wake up. This is caused by the breathing tube that was placed in your throat while you were asleep.
Pain immediately following radiofrequency ablation can be controlled by pain medication given through your IV or by injection. Afterward any mild discomfort you experience can be controlled by oral pain medications. Patients may feel nauseous, but this can also be relieved by medication.
You will remain in the recovery room until you are completely awake and ready to return home.
You should be able to resume your usual activities within a few days.
Only about ten percent of patients will still have pain a week following radiofrequency ablation.
Who interprets the results and how do I get them?
Computed tomography (CT) or magnetic resonance imaging (MRI) of the liver is performed within a few hours to a month following radiofrequency ablation. A radiologist will interpret these CT or MRI scans to detect any complications, to ensure that all of the tumor tissue has been treated and to assess any residual tumor.
You will undergo CT or MRI scans every three to four months to check for new tumors.
What are the benefits vs. risks?
Benefits
- Radiofrequency ablation can be an effective treatment for primary liver cancer and for cancers that have spread to the liver in select patients whose liver tumors are unsuitable for surgical resection.
- In most studies, more than half of the liver tumors treated by radiofrequency ablation have not recurred. The success rate for completely eliminating small liver tumors is greater than 85 percent.
- Treatment-related serious complications are infrequent and discomfort is minimal.
- Radiofrequency ablation may be used repeatedly to treat recurrent liver tumors.
- The percutaneous method of radiofrequency ablation, in which electrodes are inserted through the skin, is minimally invasive, produces few complications, and does not require hospital admission.
- RFA is a relatively quick procedure and recovery is rapid so that chemotherapy may be resumed almost immediately in patients who need it.
- Radiofrequency ablation is less expensive than other treatment options.
- No surgical incision is needed—only a small nick in the skin that does not have to be stitched.
Risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
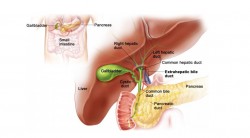
- Depending on the site of treatment, radiofrequency ablation may cause brief or, rarely, long-lasting shoulder pain; inflammation of the gallbladder that subsides after a few weeks; damage to the bile ducts resulting in biliary obstruction; or thermal damage to the bowel.
- Roughly one in four patients may develop a "post-ablation syndrome" with flu-like symptoms that appear three to five days after the procedure and usually last about five days. An occasional patient may remain ill for two to three weeks.Acetaminophen or ibuprofen taken by mouth is commonly used to control fever and other symptoms.
- Some cases of bleeding have been reported but it usually stops on its own. If bleeding is severe, an additional procedure or surgery may be needed to control it.
- Organs and tissues near the liver, such as the gallbladder, bile ducts, diaphragm and bowel loops, are at risk of being injured. Although this occurs only 3 to 5 percent of the time, it may require surgical correction. The risk of this complication is related to the location of the liver tumor that is treated.
- Less than one percent of patients may develop a localized infection (abscess) at the site of the tumor ablation three to four weeks after the treatment. A liver abscess will require tube drainage and antibiotics to cure. Patients who have had a surgical procedure in which the liver bile duct has been connected to a loop of bowel are at much greater risk of developing a liver abscess after ablation.
- Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant. See theSafety page for more information about pregnancy and x-rays.
- This procedure may involve exposure to x-rays. However, radiation risk is not a major concern when compared to the benefits of the procedure. See the Safety page for more information about radiation dose from interventional procedures.
- Severe pain after RFA is uncommon, but may last a few days and require a narcotic for relief.
What are the limitations of Radiofrequency Ablation of Liver Tumors?
There is a limit to the volume of tumor tissue that can be eliminated by radiofrequency ablation. This is due to limitations with current equipment. Hopefully technical advances will permit larger tumors to be treated in the future. Radiofrequency ablation also cannot destroy microscopic-sized tumors and cannot prevent cancer from growing back.



Leave a Reply
Want to join the discussion?Feel free to contribute!