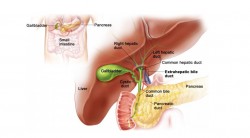
Biliary interventions treat blockages, narrowing and/or injury of the passages between the liver, gallbladder and small intestine called bile ducts. Bile is produced in the liver and stored in the gallbladder where it can be released into the small intestine to aid in digestion. If the bile ducts become blocked, it may lead to inflammation or infection also known as cholecystitis. Biliary interventions may remove gallstones, drain excess bile or place a stent within a bile duct to treat your condition and restore the flow of fluids.
Your doctor will instruct you on how to prepare based on your specific procedure and may prescribe an antibiotic. Tell your doctor about any recent illnesses or medical conditions and whether you have any allergies, especially to anesthesia or iodinated contrast material. Discuss any medications you’re taking, including herbal supplements and aspirin. You may be told not to eat or drink for several hours beforehand and advised to stop taking aspirin or blood thinner three days prior to your procedure. Leave jewelry at home and wear loose, comfortable clothing. You may be asked to wear a gown. Ask your doctor if you will be admitted to the hospital. If not, you should plan to have someone drive you home.
What are Biliary Interventions?
Biliary interventions are minimally invasive procedures performed to treat blockages or narrowing and injury of bile ducts. In addition, minimally invasive techniques can be used to treat an inflamed or infected gallbladder.
Bile, a fluid that helps digest fat in foods, is produced in the liver and flows through ducts or tubular passageways leading to thegallbladder where it is stored. When needed, the gallbladder contracts and releases bile through ducts into the small intestine.
If the bile ducts become blocked, bile cannot pass into the intestine and this may result in jaundice (in which the level of bile products in the blood becomes elevated). If the jaundice becomes severe, the patient will appear to have a yellowish hue, particularly in the whites of the eye. If the duct that connects the gallbladder to the rest of the bile ducts becomes blocked (usually due to gallstones in the gallbladder), this results in inflammation or infection (cholecystitis). This is generally treated by surgical removal of the gallbladder — either laparoscopically (minimally invasive) or by conventional open surgery. However, when patients are too ill to undergo surgical cholecystectomy, a percutaneous cholecystectomy (placement of a small tube through the skin into the gallbladder) may be performed by an interventional radiologist.
Biliary interventions include:
- Percutaneous transhepatic cholangiography (PTC), an x-ray procedure that involves the injection of a contrast materialdirectly into the bile ducts inside the liver to produce pictures of the bile ducts. This procedure is usually performed by an interventional radiologist. If a blockage or narrowing is found, additional procedures may be performed, including:
- insertion of a catheter to drain excess bile out of the body.
- removal of gallstones, stone-like objects that form in the gallbladder or bile ducts.
- stent placement, in which a small plastic or metal tube is placed inside a duct to help it remain open or to bypass an obstruction and allow fluids to drain internally.
- Endoscopic retrograde cholangiopancreatography (ERCP), a diagnostic test that combines endoscopy, which uses an illuminated optical instrument to examine inside the body, with x-ray images. This procedure is usually performed by a gastroenterologist. If a blockage or narrowing is found, additional procedures may be performed, including:
- insertion of a catheter to drain excess bile out of the body.
- removal of gallstones, stone-like objects that form in the gallbladder or bile ducts.
- sphincterotomy, in which a small incision is made in the opening of the bile duct to allow bile and small gallstones to drain.
- stent placement, in which a small plastic or metal tube is placed inside a duct to help it remain open or to bypass an obstruction and allow fluids to drain internally.
- Laparoscopic cholecystectomy, or gallbladder removal. This procedure is usually performed by a surgeon.
- Percutaneous cholecystostomy, a minimally invasive procedure in which a tube is placed in the gallbladder under imaging guidance in order to decompress a distended, inflamed and usually infected gallbladder. This procedure is typically done in patients who are too ill to undergo cholecystectomy. It is usually performed by an interventional radiologist.
An interventional radiologist is a radiologist who performs minimally invasive procedures with imaging guidance. He/she is trained in the use of fluoroscopy, CT, and ultrasound to guide passage through the skin by needle puncture, including introduction of catheters and wires for performing procedures such as biopsies, draining fluid collections or abscesses, inserting drainage catheters and dilating or stenting narrowed ducts or vessels.
What are some common uses of the procedures?
There are several conditions that can cause a blockage or narrowing in bile duct, including:
- inflammation - pancreatitis (inflammation of the pancreas), sclerosing cholangitis (inflammation of the bile ducts)
- tumors - cancer of the pancreas, gallbladder, bile duct, liver, or enlarged lymph nodes due to a variety of different tumors
- gallstones, either in the gallbladder or in the bile ducts
- injury to the bile ducts during surgery
- infection
In general, PTC and ERCP can be used to treat all of the above causes of bile duct blockage or narrowing except for actual removal of the gallbladder — this requires surgery (cholecystectomy).
How should I prepare?
Patients are routinely given antibiotics prior to this procedure.
You might have blood drawn prior to your procedure.
Prior to your procedure, your blood may be tested to determine how well your kidneys are functioning and whether your blood clots normally.
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials containing iodine (sometimes referred to as "dye" or "x-ray dye"). Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners for a specified period of time before your procedure.
Also inform your doctor about recent illnesses or other medical conditions.
Women should always inform their physician and x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
You will receive specific instructions on how to prepare, including any changes that need to be made to your regular medication schedule.
Other than medications, you may be instructed to not eat or drink anything for several hours before your procedure.
You may be asked to remove some or all of your clothes and to wear a gown during the exam. You may also be asked to remove jewelry, eye glasses and any metal objects or clothing that might interfere with the x-ray images.
You should plan to have a relative or friend drive you home after your procedure.
Some biliary interventions require an overnight stay at the hospital.
What does the equipment look like?
In this procedure, x-ray equipment, ultrasound or CT scanning may be used for image guidance. In addition, additional equipment such as an endoscope, laparoscope, catheter, balloon and/or stent may be used.
X-ray equipment:
The equipment typically used for this examination consists of a radiographic table, one or two x-ray tubes and a television-like monitor that is located in the examining room. Fluoroscopy, which converts x-rays into video images, is used to watch and guide progress of the procedure. The video is produced by the x-ray machine and a detector that is suspended over a table on which the patient lies.
Ultrasound:
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer that is used to scan the body and blood vessels. The transducer is a small hand-held device that resembles a microphone, attached to the scanner by a cord. The transducer sends out high frequency sound waves into the body and then listens for the returning echoes from the tissues in the body. The principles are similar to sonar used by boats and submarines.
The ultrasound image is immediately visible on a nearby screen that looks much like a computer or television monitor. The image is created based on the amplitude (strength), frequency and time it takes for the sound signal to return from the patient to the transducer.
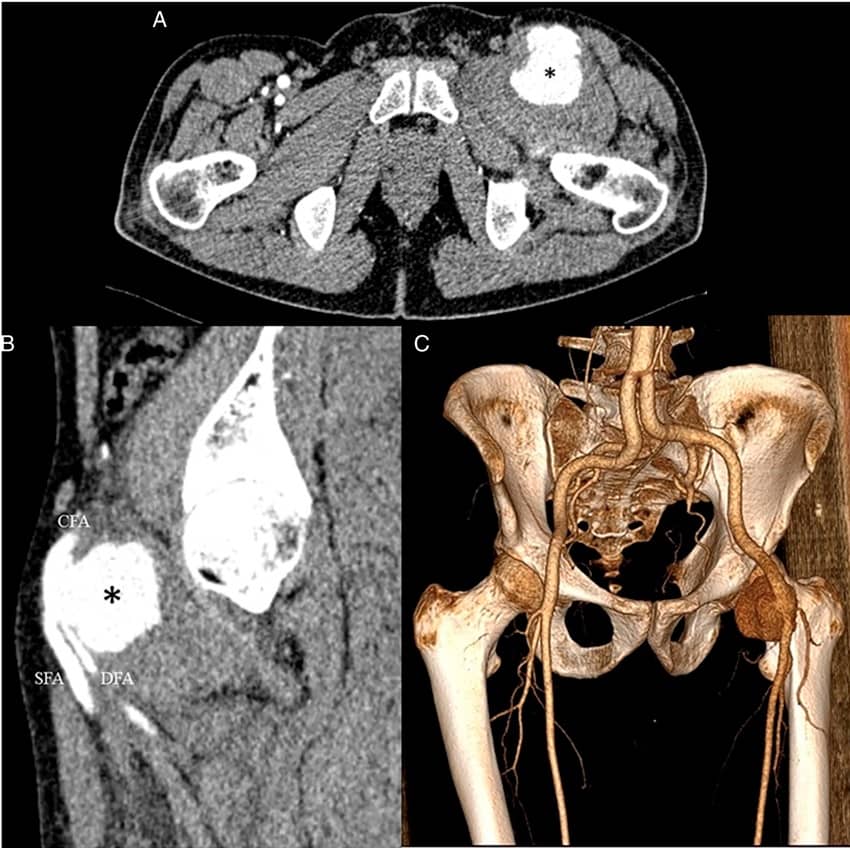
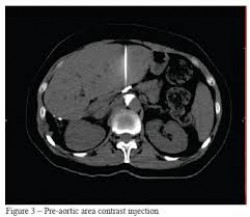
CT:
The CT scanner is typically a large, box like machine with a hole, or short tunnel, in the center. You will lie on a narrow examination table that slides into and out of this tunnel. Rotating around you, the x-ray tube and electronic x-ray detectors are located opposite each other in a ring, called a gantry. The computer workstation that processes the imaging information is located in a separate room, where the technologist operates the scanner and monitors your examination. The CT scanner obtains x-ray “slices” of your body as the gantry moves you through the scanner. These slices are typically between 0.1 and 1 cm thick.
Additional equipment:
- Catheter: a long, thin plastic tube, about as thick as a strand of spaghetti.
- Balloon: a long, thin plastic tube with a small balloon at its end.
- Stent: a small, wire mesh or plastic tube.
- Endoscope: an illuminated optical instrument used to examine inside the body.
- Laparoscope: a thin, tube-like instrument with a light and a lens for viewing the inside of the abdominal cavity.
How does the procedure work?
PTC (percutaneous transhepatic cholangiography) uses image-guidance to inject contrast material into the bile ducts to provide x-ray images of the bile ducts and gallbladder.
ERCP (endoscopic retrograde cholangiopancreatography) combines endoscopy and x-rays to examine the inside of the bile ducts, gallbladder, and pancreatic duct and to produce pictures of these on x-ray images.
Percutaneous cholecystostomy places a tube in an infected or inflamed gallbladder using imaging guidance. This serves to promote drainage of bile from the gallbladder.
Laparoscopic cholecystectomy is a procedure in which a laparoscope, a thin tube-like instrument with an attached light and a lens, is inserted through a small incision near the belly button and inserted into the abdominal cavity. The inside of the abdomen can thus be visualized on a television screen. The gallbladder is mobilized under laparoscopic guidance and removed through the small incision. If the laparoscopic approach is not possible, open surgical removal of the gallbladder would be performed.
How is the procedure performed?
These procedures may be done on an outpatient basis. However, some procedures may require admission. Please consult with your physician.
Prior to your procedure, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) may be performed.
You may be given medications to help prevent nausea and pain, and antibiotics to help prevent infection.
You will be positioned on the examining table.
You may be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedative medication can be given intravenously. Moderate sedation may be used. As an alternative, you may receive general anesthesia.
If you receive a general anesthetic, you will be unconscious for the entire procedure, and you will be monitored by ananesthesiologist.
ERCP (endoscopic retrograde cholangiopancreatography):
An endoscope is passed through the mouth, esophagus, stomach and into the first part of the small intestine. A catheter is then inserted through the endoscope and a contrast material is injected into the biliary ducts. X-rays are then taken.
PTC (percutaneous transhepatic cholangiography):
The area of your body where the needle or laparoscope is to be inserted will be shaved, sterilized and covered with a surgical drape.
A very small skin incision is made at the site.
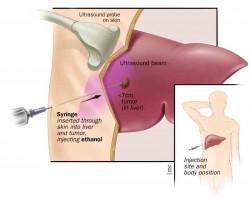
A thin needle is inserted through the skin below the ribs and into the liver using x-ray (fluoroscopy) guidance. A contrast material is injected into the liver and bile ducts and x-rays are taken. If a blockage is found, a catheter may be temporarily left in the liver to drain bile into the small intestine or a collection bag outside the body.
Stent placement: using image-guidance, a stent may be placed in a narrow portion of a bile duct to help keep the duct open. A balloon-tipped catheter may be used to help expand a narrow duct.
Stents can be self-expandable (opens up itself upon deployment) or balloon expandable (balloon needed to open the stent). Balloon expandable stents are typically placed over a balloon-tipped catheter so that when the balloon is expanded, it pushes the stent in place against the duct wall. When the balloon is deflated and removed, the stent remains in place, acting like a scaffold for the duct.
Gallstone removal: if imaging reveals a gallstone in the common bile duct (CBD), the doctor may make a small incision in the bile duct and remove the stone(s).
Laparoscopic cholecystectomy:
A laparoscope, a thin tube-like instrument with an attached light and a lens, is inserted through a small incision near the belly button. The abdomen is inflated with carbon dioxide to provide a better view of the operative area. Three additional incisions are made near the laparoscope through which special surgical instruments are inserted. Guided by the internal images obtained by the laparoscope that are projected onto video monitors, the physician removes the gallbladder.
Your intravenous line will be removed.
What will I experience during and after the procedure?
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected. Most of the sensation is at the skin incision site which is numbed using local anesthetic. You may feel pressure when the catheter is inserted into the vein or artery.
If you receive a general anesthetic, you will be unconscious for the entire procedure, and you will be monitored by ananesthesiologist.
If the procedure is done with sedation, the intravenous (IV) sedative will make you feel relaxed and sleepy. You may or may not remain awake, depending on how deeply you are sedated.
As the contrast material passes through your body, you may get a warm feeling.
You will remain in the recovery room until you are completely awake and ready to return home.
In general, for all of these procedures, you should be able to resume your normal activities within a few days. In some cases, you may have a catheter exiting your side and draining bile into a bag. The duration of the drainage into a bag will vary from patient to patient. Consult your interventional radiologist for information about your treatment.
Who interprets the results and how do I get them?
The interventional radiologist or physician treating you will determine the results of the procedure and will send a report to your referring physician, who will share the results with you.
Your interventional radiologist may recommend a follow-up visit after your procedure or treatment is complete.
The visit may include a physical check-up, imaging procedure(s) and blood or other lab tests. During your follow-up visit, you may discuss with your doctor any changes or side effects you have experienced since your procedure or treatment.
What are the benefits vs. risks?
Benefits
- For PTC and related procedures no surgical incision is needed—only a small nick in the skin that does not have to be stitched closed. For ERCP and related procedures, no surgical incision is needed. For laparoscopic procedures, only small incisions are needed.
- The additional risks of open surgery are avoided.
- The period of hospitalization in general is less than for open surgery.
- Recovery time is significantly shorter than open surgery.
Risks
- Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
- There is a very slight risk of an allergic reaction if contrast material is injected.
- There is a small risk of bleeding related to the procedure. If this occurs, this is almost always self limiting. If treatment becomes necessary, this can almost always be achieved with arterial embolization, a minimally invasive technique.
- There is a very small risk of organ damage, such as bowel perforation.
What are the limitations of Biliary Interventions?
Minimally invasive procedures such as biliary interventions may not be appropriate for all patients. The decision as to whether your specific situation can be treated with these techniques will be made by your physician and interventional radiologist. As a general rule, minimally invasive procedures are preferable to open surgery but there are instances in which a minimally invasive procedure would not be appropriate. In general, if this were the case, open surgery would be the procedure of choice.
In some cases, a recurrence of the underlying problem such as blockage of a stent or cholecystitis may occur. In these cases, repeat biliary intervention may be necessary. If this were not felt to be appropriate, open surgery could be performed.



Leave a Reply
Want to join the discussion?Feel free to contribute!